The effect of hypnotherapy on the quality of life in women with breast cancer
Abstract
Background. Cancer is a chronic disease that significantly affects the quality of life of patients who suffer from it, because they must face stressful situations, including their diagnosis, surgical procedures, and the adverse effects of chemotherapy and radiotherapy.
Objective. To evaluate the effects of hypnotherapy on breast cancer patients’ quality of life during chemotherapy.
Design. A quasi-experimental design was used with a convenience sample. Method. Two groups of patients with early breast cancer diagnoses were assigned to either a control group that received standard medical care (n = 20), or a hypnotherapy group (n = 20) that received 12 intensive sessions over the course of 1 month, and 12 additional sessions over the course of 6 months. The patients’ quality of life was evaluated using the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30).
Results. The hypnotherapy group showed a statistically significant improvement and a large effect size on the cognitive functioning and social functioning scales compared to the control group. The physical functioning, role functioning, and quality of life scales showed improvement with a medium effect size, but the changes were not statistically significant.
Conclusion. The improvement observed in the cognitive functioning and social functioning scales allows us to suggest that hypnotherapy improves the quality of life of breast cancer patients during chemotherapy.
Received: 18.08.2016
Accepted: 18.04.2017
Themes: Clinical psychology
PDF: http://psychologyinrussia.com/volumes/pdf/2017_2/psych_2_2017_16.pdf
Pages: 228-240
DOI: 10.11621/pir.2017.0216
Keywords: hypnotherapy, quality of life, breast cancer, cognitive functioning and social functioning
Introduction
According to the World Health Organization (WHO, 1948), health is a state of full physical, mental, and social well-being, not simply the absence of an illness or ailment. By contrast, quality of life refers to general well-being, including physical, psychological, social, economic, and political features (Revicki et al., 2000).
Health-Related Quality of Life (HRQOL) describes the quality of life of people who suffer from a specific illness, generally one that is chronic. Quality of life in these cases is affected by the debilitating consequences of the illness itself, or by the side effects of medical treatment. HRQOL can be defined as a subjective and multidimensional state that encompasses physical, occupational, emotional, social, and cognitive functioning, as well as levels of vitality, pain, sexuality, and spirituality (Osoba, 2011).
Cancer is a chronic disease that significantly affects the quality of life of patients who suffer from it because they must face stressful situations, including their diagnosis, surgical procedures, and the adverse effects of chemotherapy and radiotherapy (Pocino et al., 2007). Women who have received medical treatment for breast cancer regularly report pain, fatigue, difficulty sleeping, nausea, vomiting, and hot flashes (Ewertz & Jensen, 2011).
Breast cancer patients’ quality of life varies according to the type of treatment. With regard to the type of surgery, radical surgery generates the greatest anxiety and self-image problems. By contrast, women who have had reconstructive and conservative surgery exhibit higher quality of life levels, particularly in dimensions such as physical functioning, emotional role, and social role (Roman, Olivares, Martin, Martin & Moreno, 2010; Royo, 2011).
Chemotherapy also negatively affects the quality of life of women who suffer from breast cancer, particularly because of the side effects that affect their physical, functional, and emotional state. Sat-Munoz et al. (2011) found that the emotional dimension was the most strongly affected in Mexican women with breast cancer.
Longitudinal studies reveal that breast cancer patients’ quality of life is affected even 6, 9 or 12 months after the patients have finished treatment. The patients’ emotional functioning, role functioning and vitality are the dimensions that deteriorate the most, along with body image and sexual, cognitive, and social functioning (Dominguez et al., 2009; Hard et al., 2010; Schou, Ekeberg, Sandvik, Hjermstad & Ruland, 2005).
Because of the negative side effects that cancer treatment tends to have, a large portion of scientific studies have focused on finding therapeutic techniques and strategies to improve HRQOL in these patients (Fayers & Bottomley, 2002).
Hypnosis is a technique that has been used over the past few centuries to treat chronic diseases, and it has had positive results in providing physical and psychological well-being for patients undergoing it (Montgomery, Schnur, & Kravits, 2013). Hypnosis has also been shown to be effective in managing various physical and psychological symptoms in breast cancer patients, including distress, anxiety, hot flashes, fatigue, quality of sleep, and pain (Elkins, Fisher, Johnson, Carpenter, & Keith, 2013; Jaime, Tellez, Juarez, Garcia, & Garcia, 2015; Montgomery et al., 2014).
Moreover, hypnosis improves the quality of life in patients with metastases (Liossi & White, 2001; Laidlaw, Bennet, Dwivedi, Nait & Gruzelier, 2005). A review by Cramer et al. (2014) confirms these findings. However, to our knowledge, the direct effects of hypnotherapy on quality of life and the elements of functioning during chemotherapy, have not been studied previously.
The purpose of this study was to determine the effects of hypnotherapy on the quality of life of women with breast cancer during chemotherapy, compared to a control group that received standard medical care.
Method
This paper is a secondary analysis of a broader study of the effects of hypnosis on the well-being of breast cancer patients, in which components of the quality-of-life variable are analyzed. The psychosocial variables studied by this team are available in another publication (Tellez et al, 2017). A quasi-experimental design was used with a convenience sample.
Participants
Fifty-six patients were invited to participate. Of these, 16 rejected the invitation. Thus 40 women with breast cancer were included in the initial stages (I, II, and III). These women had no metastases, no prior cancers, no previous participation in hypnotherapy, and were scheduled to receive chemotherapy within the following 2 weeks. In the second phase of the study, 4 patients left the study voluntarily: 2 from the intervention group and 2 from the control group.
In terms of socio-demographic characteristics, the median age was 52 years for the intervention group and 52.2 years for the control group. With regard to the marital status of the hypnotherapy group, 10% were single, 45% were married, 15% were in a domestic partnership, 15% were separated, and 15% were widowed. In the control group, 15 % were single, 65 % were married, 5 % were in a domestic partnership, 10% were separated, and 5% were widowed. All those in the hypnotherapy group and 85 % of those in the control group had children. With regard to socioeconomic status, the intervention group was 55% lower class and 45 % middle-class, whereas the control group was 25 % lower-class and 75% middle-class.
Procedure
This study was performed in Mexico, and was approved by the ethics committee in Health Science of Universidad Autonoma de Nuevo Leon. All of the participants signed an informed consent form prior to beginning the procedure.
The 40 patients were referred by an oncologist who was part of the research group. The first 20 patients referred were assigned to the hypnotherapy intervention group, and the next 20 patients were assigned to the control group with standard medical care only.
The intervention consisted of 24 hypnotherapy sessions, each lasted 90 minutes, and was divided into 2 phases. The first phase involved 12 intensive sessions, with a frequency of 3 sessions per week, over the course of 1 month. The second phase involved 12 sessions, with a frequency of 1 session fortnightly, for 6 months. These sessions occurred throughout the chemotherapy treatment.
Evaluations were conducted before treatment, and at the end of the first and second phase. Evaluations of the control group were conducted in tandem with the evaluations of the intervention group.
Hypnotherapeutic intervention
Hypnotic intervention: In each session, a suggestive technique was used targeting specific symptoms for an average of 20 minutes. After the first hypnotic induction, a 10-minute pause was taken to discuss the experience, and have the patients rated their feeling of relaxation on a visual analogue scale from 1 to 10.
Second hypnotic technique: The Battino and South (2005) technique was used in the 24 sessions, This technique consists of taking the patients hand and giving her a series of suggestions directed at strengthening the immune system.
Each of the patients in the hypnotherapy group received MP3 equipment to listen to the hypnotherapy techniques at home.
In Phase 1, two sessions focused on physical and psychological relaxation (Field, 1990), and one session focused on facilitating sleep and relaxation (Tellez, 2007). Three sessions focused on strengthening self-esteem (Pelletier, 1979; Torem, 1990; Cobian, 1997), four sessions focused on resolving traumatic events from the past (Watkins & Watkins, 1990; Watkins, 1980; Wright, 1987; Greenberg & Malcolm, 2002), one session focused on physical healing (Dilts, Smith, Halbom &, 1998), and one session was directed at increasing optimism (Korn & Pratt, 1990).
In Phase 2, five sessions were focused on physical healing (Hammond, 1990), two on physical and psychological relaxation (Hammond, 1990; Sacerdote, 1977), two sessions focused on strengthening self-esteem (Gorman, 1974; Pekala & Kumar, 1999), two sessions were used to strengthen positive expectations and motivation for change (Hammond, 1990; Tellez, 2007), and another session was used to facilitate sleep and relaxation (Stanton, 1990).
Measures
The quality of life evaluation was performed using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQC30), which is an integrated system used to evaluate the quality of life of patients with cancer diagnoses. The EORTC QLQ-C30 consists of 30 items, 24 of which are organized into 9 multi-item scales that represent various dimensions of quality of life: an overall scale; 5 functioning scales (physical, role, emotional, cognitive, and social); and 3 scales to measure symptoms (fatigue, pain, and nausea) (Aaronson et al., 1993). The EORTC QLQ-C30 is considered to be highly sensitive in detecting changes in well-being in cancer patients during chemotherapy (Uwer et al., 2011).
Data analysis
The data were analyzed using SPSS Statistics V. 21.0. A one-way analysis of variance (ANOVA) with a change score was used, as recommended by Huck and McLean (1975), to adjust any possible differences in the pre-test evaluation. Additionally, the size effect was obtained using the formula for pretest/post-test designs with a control group, using the adjustment to reduce bias (Morris, 2008). The confidence intervals for effect size were obtained using the Campbell collaboration online calculator (Lipsey & Wilson, 2001).
The clinical significance, or practical value, of hypnotherapy was judged by evaluating the size of its effect according to the Cocks et al. (2011) guide. These authors established guidelines for evaluating differences between QLQ-C30 scores. The authors used 4 effect size categories: large (1) = unequivocal clinical relevance; medium (m) = clinical relevance is probable, but to a lesser degree; small (s) = a change that is subtle but clinically relevant; and trivial = situations that are unlikely to have clinical relevance, or in which there were no differences. Likewise, the authors note that these effects sizes are different in each functioning scale: cognitive 3-9 (s), 11-15 (m), and >15 (I); physical 5-14 (s), 14-22 (m), and >22 (1); role 6-19 (s), 19-29 (m), and >29 (1); social 5-11 (s), 11-15 (m), and >15 (1); and overall quality of life 4-10 (s), 10-15 (m), and >15 (1).
Results
By group
In the first month of intensive treatment, significant differences were observed in the hypnotherapy group, with regard to the scales for physical and social functioning and overall quality of life. The last 2 scales showed a large effect size.
After 6 months, the most notable changes were observed on the scales for cognitive functioning (p = 0.011, d = 1.18) and the social functioning scale (p = 0.015; d= 1.02), with a large effect size.
Regarding physical functioning, a large effect size was observed (d = 0.91), whereas for role functioning (d = 0.58) and overall quality of life (d = 0.51), a medium effect size was observed, but this was not statistically significant (Table 1). Therefore, if there is a therapeutic effect, its statistical significance would have to be achieved by increasing the sample size (statistical power) (Tellez, Garcia & Corral, 2015).
On the symptom scales, although the patients in the intervention group showed a greater reduction in symptoms, the changes were not significant (Table 2).
Analysis using the Cocks et al. (2011) guide
According to the Cocks et al. (2011) interpretation guide, the scores obtained by the hypnotherapy group revealed an improvement with a small effect size in regard to social functioning at the end of the first month, and at the end of 6 months (8.5 and 10 points, respectively). An improvement was obtained in regard to overall quality of life, with a medium effect size at the end of 1 month (13 points), and a small effect size at the end of 6 months (6 points). Hypnotherapy had a trivial effect on cognitive functioning during the first month; however, there was an improvement with a large effect at the end of 6 months (19 points) (Figure 1).
The control group scores illustrated deterioration in various scales. Cognitive functioning exhibited deterioration with a small effect size after 1 month and after 6 months (-3 and -6 points, respectively). Social functioning also exhibited dete rioration, with a small effect size after 1 month (-11) and a large effect size after 6 months (-19). Overall quality of life deteriorated with a small effect size after the first month and after 6 months (-5.8 and -5.3, respectively).
Table 1. Change scores for the QLQ-30 functionality subscale.
|
QLQ-C30 |
|
Intensive Treatment 1 Month |
|
Regular Treatment 6 Months |
||||
|
Subscale |
CSM Hypnosis |
CSM Control |
F value (p) |
d [95% Cl] |
CSM Hypnosis CSM Control |
F value (p) |
d [95% Cl] |
|
|
Physical Functioning |
4.9 (15.2) |
-3.3 (8.8) |
4.36 (0.43)* |
0.42 [-0.21,1.00] |
0 (16.3) |
-15.6 (30.2) |
3.69 (0.063) |
0.91 [-0.20,1.60] |
|
Role Functioning |
5 (30.1) |
-0.83 (23.2) |
0.469 (0.497) |
0.21 [-0.41, 0.83] |
5.5 (30.7) |
-8.8 (41.2) |
1.37 (0.249) |
0.58 [-0.09,1.25] |
|
Emotional Functioning |
14.5 (17.9) |
13.7 (22.6) |
0.017 (0.898) |
0.04 [-0.58, 0.66] |
13.8(18.9) |
11.2 (26.1) |
0.115(0.736) |
-0.14 [-0.80, 0.52] |
|
Cognitive Functioning |
0.83 (15.7) |
-3.3(19.1) |
0.563 (0.457) |
0.19 [-0.43, 0.81] |
19.1 (20.5) |
-6.8 (35.2) |
7.16 (0.11)* |
1.18 [-0.45,1.89] |
|
Social Functioning |
8.5 (30.6) |
-11.2(18.5) |
6.11 (0.18)* |
0.83 [0.17,1.50] |
10.1 (30.3) |
-19.6 (38.2) |
6.55 (0.15)* |
1.02 [0.30,1.71] |
|
Global QoL |
13.3 (26.6) |
-5.8 (29.9) |
5.19 (0.28)* |
1.0 [0.33,1.60] |
6.9 (23.2) |
-5.3 (25.5) |
2.23 (0.144) |
0.51 [-0.12,1.14] |
Table 2. Score changes in the symptoms subscale of the QLQ-30
|
Symptoms QLQ |
|
Intensive Treatment 1 Month |
|
Regular Treatment 6 Months |
||||
|
Hypnosis |
Control |
F(p) |
d(IC) |
Hypnosis |
Control |
F(p) |
d(IC) |
|
|
Fatigue |
-9.4(17.3) |
-2.2 (20.2) |
1.46 (0.234) |
0.38 [-0.24,1] |
3.7 (17.4) |
17.4 (35.5) |
0.978 (0.330) |
0.33 [-0.33,1.0] |
|
Nausea/Vomiting |
1.6 (15.7) |
8.2 (20.3) |
1.29 (0.262) |
0.35 [-0.26, 0.79] |
1.8 (17.9) |
1.9 (10.0) |
0.002 (0.964) |
0.01 [-0.64, 0.67] |
|
Pain |
-7.5 (21.2) |
-5.8 (19.7) |
0.066 (0.799) |
0.25 [-0.36, 0.87] |
0.92 (28.8) |
3.9 (34.6) |
0.000 (0.990) |
0 [-0.66, 0.66] |
|
Dyspnea |
-8.2 (14.6) |
-1.7 (31.3) |
0.717 (0.402) |
0.26 [-0.35, 0.89] |
5.5 (23.5) |
7.8 (27.2) |
0.097 (0.758) |
0.1 [-0.55, 0.76] |
|
Insomnia |
-13.3 (41) |
-6.6 (35.2) |
0.304 (0.585) |
0.17 [-0.44,0.79] |
-5.5 (52.7) |
3.9 (52.5) |
0.040 (0.843) |
0.21 [-0.45,0.87] |
|
Loss of appetite |
-1.6 (19.9) |
2.2 (24) |
0.312 (0.580) |
0.17 [-0.44,0.79] |
16.6 (28.5) |
3.9 (38.8) |
1.11 (0.299) |
0.35 [-0.31,1.02] |
|
Constipation |
-6.4 (22.5) |
-4.9 (30.7) |
0.031 (0.861) |
0.17 [-0.44,0.79] |
-5.5 (23.5) |
12.5 (36.2) |
3.03 (0.091) |
0.58 [-0.08,1.26] |
|
Diarrhea |
-1.6 (14.7) |
2.2 (32.5) |
.0136 (0.715) |
0.11 [-0.5, 0.79] |
24(19.1) |
9.8 (28.2) |
3.63 (0.065) |
0.64 [-0.03,1.3] |
The effect of hypnotherapy on the quality of life in women with breast cancer
Abbreviations: CSM — change score mean; d = effect size or the standardized mean difference; SD — standard deviations; Cl — confidence interval at 95 %; p — significance level; QoL — quality of life
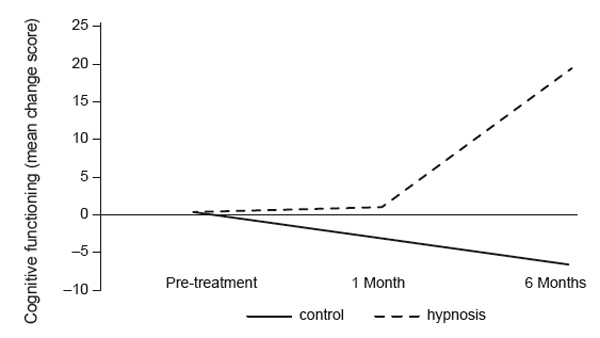
Figure 1. Mean score change in cognitive functioning (QLQ-C30) measured at baseline and after 1 and 6 months in hypnotherapy and control conditions. This figure shows an improvement in cognitive functioning in the hypnosis group and a decline in the control group.
Analysis by the number of patients with clinical changes The results obtained here were similar to the analyses of the group scores. After 6 months, the patients in the control group worsened nearly 8 times more (6 vs 47%) (p = 0.003, d= 1.04) in terms of cognitive functioning, and 3 times more in terms of social functioning and overall quality of life, than those undergoing hypnotherapy. All of these factors had a large effect size and were statistically significant. The control group also had a higher number of patients whose physical and role functioning worsened, with a medium effect size that was not statistically significant. No changes were observed with regard to emotional functioning (Table 3).
Table 3. Proportion of patients whose scores worsened on the QLQ-C30 scales (decline in the effect size of d < 0.50).
|
QLQ-C30 Functioning Scale |
% Px Worsened Hypnosis |
% Px Worsened Control |
p-value |
Effect size (Cohen's d) |
|
Physical |
22 |
59 |
0.11 |
0.66* |
|
Role |
28 |
47 |
0.12 |
0.54* |
|
Emotional |
16 |
11 |
0.38 |
0.43 |
|
Cognitive |
6 |
47 |
0.003 |
1.04** |
|
Social |
17 |
59 |
0.03 |
0.80** |
|
Global QoL |
11 |
41 |
0.05 |
0.80** |
Medium effect size ** Large effect size. Px: patient
Discussion
This study shows that 24 group hypnotherapy sessions over a period of 6 months improved the quality of life for women with breast cancer during chemotherapy treatment. In the three analyses performed, the functioning scales that showed improvement occurred for social, physical, and cognitive functioning, and for overall quality of life based on the QLQ-C30, with medium to large effect sizes. The scales for emotional functioning, role, and symptoms did not reveal significant differences.
The use of different types of analysis, such as Fisher s exact test to measure the number of patients who improve or worsen, as well as the interpreting of QLQC30 scores using the Cocks et al. (2011) guide, allowed us to determine whether the treatment, in this case hypnotherapy, makes a real or palpable difference in the patients daily life (Kazdin, 1999).
One of the most notable effects of hypnotherapy was the improvement in cognitive functioning. Cognitive alterations are among the most common symptoms related to cancer (Janelsins et al., 2011). Evaluations of overall cognitive functioning as well as immediate free recall, delayed memory, verbal memory, selective attention, attention span, and abstract reasoning indicate deterioration during and after breast cancer-treatment-related procedures (Lindner et al., 2014; Biglia et al., 2012; Vearncombe et al., 2009; Ando-Tanabe et al., 2014).
Hartl et al., (2010) found out that after a mastectomy and with the passage of time, all QLQ-C30 functioning scales improve, except cognitive functioning. Indeed, these cognitive deficits can be detected up to 20 years after having finished chemotherapy (Koppelmans et al., 2012).
Although evidence exists of cognitive alterations produced by medical treatment in patients with breast cancer, few studies have demonstrated the effectiveness of psychological techniques in improving or preventing cognitive decline in these patients. Some of the strategies that have demonstrated effectiveness in improving cognitive alterations related to chemotherapy include cognitive training (King & Green, 2015) and neuropsychological rehabilitation (Poppelreuter, Weis, & Bartsch, 2009). However, our study provides the first evidence that hypnotherapy has a positive effect on self-reported cognitive functioning, which suggests that hypnotherapy can be a useful tool in avoiding cognitive decline in patients with cancer. However, it would be advisable to use specific neuropsychological tests to confirm this finding.
Furthermore, although some studies have found that social functioning is not affected during chemotherapy (Recalde & Samudio, 2012; Denieffe, Cowman, & Gooney, 2013), in this study, the control group declined by 20 points on this scale, whereas the hypnotherapy group improved by 10 points. In other words, there was a difference of almost 30 points between the 2 groups. Richardson et al. (1997) also reported an improvement in this type of functioning using guided imagery. Efficace et al. (2006) highlight the importance of social functioning because it is a predictive factor in cancer patient survival.
Likewise, in the hypnotherapy group, trivial changes were observed in physical functioning after the first month, and no changes were observed after 6 months, whereas the control group worsened in this aspect. This indicates that hypnotherapy patients maintained their normal level of physical functioning in spite of the chemotherapy treatment, and, as Kazdin (1999) has noted, a small change, and even a lack of change, can be clinically relevant.
Physical functioning is important because it allows patients to achieve a certain level of independence in performing their day-to-day activities, including getting out of bed, dressing, and eating. It also increases the likelihood that the patient will be able to reintegrate into work and social life, and improve her quality of life (Campbell et al., 2012).
Compared to the control group, the overall quality of life of patients in the intervention group improved. This is important because the perception of overall quality of life implies a sense of general well-being for patients in their daily lives (Bellver, 2007). Overall quality of life is one of the main factors taken into consideration in developing and implementing effective interventions to promote wellbeing and reduce the individual and social effects of cancer (Weaver et al., 2012). As such, hypnotherapy can be considered an intervention that promotes quality of life and the perception of well-being in patients with breast cancer.
In regard the role and emotional functioning scales, in the former we observed small changes, although they were not significant, whereas no changes were observed in terms of emotional functioning. One possible explanation for this result could be that this scale was considered informative by the patients reporting, and was not very sensitive to clinical changes (Cocks et al., 2011).
Conclusion
This study described the benefits of hypnotherapy for the quality of life of women with cancer who receive chemotherapy. However, it ought to be mentioned that the convenience sampling, the small sample size, and the lack of follow-up limit the generalizability of the results. For this reason, we suggest that a randomized clinical trial be performed with follow-up and sufficient statistical power to confirm these results. Additionally, it is important to use specific instruments to evaluate the different scales. For example, it is necessary to use neuropsychological tests to measure cognitive functioning, rather than rely on self-reporting.
This study offers preliminary evidence of the utility of hypnotherapy during chemotherapy in increasing cognitive functioning and reducing adverse effects on social and physical functioning and overall quality of life in women with breast cancer.
References
Aaronson, N.K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, & Kaasa, S. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365-376. doi: 10.1093/jnci/85.5.365
Ando-Tanabe, N., Iwamitsu, Y., Kuranami, M., Okazaki, S., Yasuda, H., Nakatani, Y, & Miyaoka, H. (2014). Cognitive function in women with breast cancer receiving adjuvant chemotherapy and healthy controls. Breast Cancer, 21(4), 453-462. doi: 10.1007/sl2282-012-0405-7
Battino, R., & South, T.L. (2005). Ericksonian approaches: A comprehensive manual. Wales, UK: Crown House Publishing.
Bellver, A. (2007). “Eficacia de la terapia grupal en la calidad de vida у el estado emocional en mujeres con cancer de mama”. Psicooncologia, 4(1), 133-142.
Biglia, N., Bounous, V.E., Malabaila, A., Palmisano, D., Torta, D.M.E., D’alonzo, M…& Torta, R. (2012). Objective and self-reported cognitive dysfunction in breast cancer women treated with chemotherapy: a prospective study. European Journal of Cancer Care, 21(4), 485-492. doi: 10.1 lll/j.1365-2354.2011.01320.x
Campbell, K.L., Pusic, A.L., Zucker, D.S., McNeely, M.L., Binkley, J.M., Cheville, A.L., & Harwood, K.J. (2012). A prospective model of care for breast cancer rehabilitation: Function. Cancer, 118(S8), 2300-2311. doi: 10.1002/cncr.27464
Cobian, M. (1997). Yo si creo en la hipnosis. Santiago de Cuba: Oriente.
Cocks, K., King, M.T., Velikova, G., St-James, M.M., Fayers, P.M., & Brown, J.M. (2011). Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Journal of Clinical Oncology, 29(1), 89-96. doi: 10.1200/JC0.2010.28.0107
Cramer, H., Lauche, R., Paul, A., Langhorst, J., Kummel, S., & Dobos, G. (2014). Hypnosis in breast cancer care: A systematic review of randomized controlled trials. Integrative Cancer Therapies, 14(1), 5-15. doi: 1534735414550035.
Denieffe, S., Cowman, S., & Gooney, M. (2013) Symptoms, clusters and quality of life prior to surgery for breast cancer. Journal of Clinical Nursing, 23(17), 2491-2502. doi: 10.1111/ jocn.12430
Dilts, R., Smith, S., & Hallbom, T. (1998). Identificacion у cambio de creencias. Barcelona: Ediciones Urano, SA.
Dominguez Gil, M.R., Acosta Mosquera, M.E., Mendez Martin, I., Maestre Ramos, I., Pedrote Ramirez, C., & Frutos Canto, M. (2009). Evaluation de la Calidad de Vida tras el tratamiento primario del cancer de mama. Index de Enfermena, 18(4), 246-248. doi: 10.4321/S113212962009000400007
Efficace, E, Bottomley, A., Smit, E.F., Lianes, P, Legrand, C., Debruyne, C.... & Meerbeeck, J.V. (2006). Is a patient's self-reported health-related quality of life a prognostic factor for survival in non-small-cell lung cancer patients? A multivariate analysis of prognostic factors of EORTC study 08975. Annals of Oncology, 17(11), 1698-1704. doi: 10.1093/annonc/mdll83
Elkins, G.R., Fisher, W.I., Johnson, A.K., Carpenter, J.S., & Keith, T.Z. (2013). Clinical hypnosis in the treatment of postmenopausal hot flashes: A randomized controlled trial. Menopause, 20(3), 291-298. doi: 10.1097/GME.0b013e31826ce3ed.
Ewertz, M., & Jensen, A.B. (2011). Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncologica, 50(2), 187-193. doi: 10.3109/0284186X.2010.533190.
Fayers, R, 8c Bottomley, A. (2002). Quality of life research within the EORTC — the EORTC QLQC30. European Journal of Cancer, 38(4), 125-133. doi: 10.1016/S0959-8049(01)00448-8
Field, E.S. (1990). Neurolinguistic programming as an adjunct to other psychotherapeutic/hypnotherapeutic interventions. American Journal of Clinical Hypnosis, 32(3), 174-182. doi: 10.1080/00029157.1990.10402822
Gorman, B.J. (1974). An abstract technique of ego-strengthening. American Journal of Clinical Hypnosis, 16(3), 209-211. doi: 10.1080/00029157.1974.10403679
Greenberg, L.S., & Malcolm, W. (2002). Resolving unfinished business: Relating process to outcome. Journal of Consulting and Clinical Psychology, 70(2), 406-416. doi: 10.1037/0022-006X.70.2.406
Hammond, D.C. (1990). Handbook of hypnotic suggestions and metaphors. New York: WW Norton & Company.
Hartl, K., Engel, J., Herschbach, R, Reinecker, H., Sommer, H., & Friese, K. (2010). Personality traits and psychosocial stress: Quality of life over 2 years following breast cancer diagnosis and psychological impact factors. Psycho-Oncology, 19(2), 160-169. doi: 10.1002/ pon.1536.
Huck, S. W. & McLean, R. A. (1975). Using a repeated measure ANOVA to analyze the data from a pretest-posttest design: A potentially confusing task. Psychological Bulletin, 82(4), 511-518. DOI: 10.1037/h0076767
Jaime Bernal, L., Tellez Lopez, A., Juarez Garcia, D.M., Garcia Cadena, C.H., & Garcia Garcia, E. (2015). El efecto de la hipnoterapia en la calidad de sueno de mujeres con cancer de mama. Psicooncologxa, 12(1), 39-49. doi: 10.5209/rev_PSIC.2015.vl2.nl.48902
Janelsins, M.C., Mustian, K.M., Peppone, L.J., Sprod, L.K., Shayne, M., Mohile, S. ... Morrow, G.R. (2011). Interventions to alleviate symptoms related to breast cancer treatments and areas of needed research. Journal of Cancer Science & Therapy, 2, S2-001. doi: 10.4172/19485956.S2-001
Kazdin, A.E. (1999). The meanings and measurement of clinical significance. Journal of Consulting and Clinical Psychology, 67(3), 332-339. doi: 10.1037/0022-006X.67.3.332
King, S. & Green, H.J. (2015). Psychological intervention for improving cognitive function in cancer survivors: A literature review and randomized controlled trial. Frontiers in Oncology, 5, 72. doi: 10.3389/fonc.2015.00072
Koppelmans, V., Breteler, M.M., Boogerd, W, Seynaeve, C., Gundy, C., & Schagen, S.B. (2012). Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. Journal of Clinical Oncology, 30(10), 1080-1086. doi: 10.1200/ JCO.2011.37.0189
Korn, E., & Pratt, G. (1990). Mental rehearsal: The protective shield. In: D. Corydon (Ed.) Handbook of hypnotic suggestions and metaphors (pp. 547). New York: W.W. Norton and Company.
Laidlaw, T, Bennet, B. M., Dwivedi, P, Naito, A., & Gruzelier, J. (2005). Quality of life and mood changes in metastatic breast cancer after training in self-hypnosis or Johrei: a short report. Contemporary Hypnosis, 22(2), 84-93. doi: 10.1002/ch.27
Lindner, O.C., Phillips, B., McCabe, M.G., Mayes, A., Wearden, A., Varese, E, & Talmi, D. (2014). A meta-analysis of cognitive impairment following adult cancer chemotherapy. Neuropsychology, 28(5), 726-740. doi: 10.1037/neu0000064
Liossi, C., & White, P. (2001). Efficacy of clinical hypnosis in the enhancement of quality of life of terminally ill cancer patients. Contemporary Hypnosis, 18(3), 145-160. doi: 10.1002/ch.228
Lipsey, M.W., & Wilson, D.B. (2001). Practical meta-analysis effect size calculator. [Online calculator] . Retrieved from: http://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD-main.php
Montgomery, G.H., David, D., Kangas, M., Green, S., Sucala, M., Bovbjerg, D.H. ... Schnur, J.B. (2014). Randomized controlled trial of a cognitive-behavioral therapy plus hypnosis intervention to control fatigue in patients undergoing radiotherapy for breast cancer. Journal of Clinical Oncology, 32(6), 557-563. doi: 10.1200/JC0.2013.49.3437
Montgomery, G., Schnur, J. & Kravits, K. (2013). Hypnosis for cancer care: Over 200 years young. Hypnosis for Cancer Care, 63(1), 31-44. doi: 10.3322/caac.21165
Morris, S.B. (2008). Estimating effect sizes from the pretest-posttest-control group designs. Organizational Research Methods, 11(2), 364-386. doi: 10.1177/1094428106291059
Organizacion Mundial de la Salud. (1948). Constitucion de la Organizacion Mundial de la Salud. Retreived from: http://apps.who.int/gb/bd/PDF/bd48/basic-documents-48th-edition-sp. pdf?ua=l#page=7
Osoba, D. (2011). Health-related quality of life and cancer clinical trials. Therapeutic Advances in Medical Oncology, 3(2), 57-71. doi: 10.1177/1758834010395342
Pekala, R.J., & Kumar, V.K. (1999). Ego strengthening protocol. Coatesville, P.A.: Coatesville VA Medical center.
Pelletier, A.M. (1979). Three uses of guided imagery in hypnosis. American Journal of Clinical Hypnosis, 22(1), 32-36. doi: 10.1080/00029157.1979.10403998
Pocino, M., Luna, G., Canelones, P, Mendoza, A., Romero, G., Palacios, L.E., Rivas, L… & Castes, M. (2007). La relevancia de la intervention psicosocial en pacientes con cancer de mama. Psicooncologta, 4(1), 59-73.
Poppelreuter, M., Weis, J., & Bartsch, H.H. (2009). Effects of specific neuropsychological training programs for breast cancer patients after adjuvant chemotherapy. Journal of Psychosocial Oncology 27(2), 274-296. doi: 10.1080/07347330902776044.
Recalde, M.T. 8c Samudio, M. (2012). Calidad de vida en pacientes con cancer de mama en tratamiento oncologico ambulatorio en el Instituto de Prevision Social en el ano 2010. Memorias del Instituto de Investigaciones en Ciendas de la Salud, 10(2), 13-29.
Revicki, D.A., Osoba, D., Fairclough, D., Barofsky, L, Berzon, R., Leidy, N.K., & Rothman, M. (2000). Recommendations on health-related quality of life research to support labeling and promotional claims in the United States. Quality of Life Research, 9(8), 887-900. doi: 10.1023/A: 1008996223999
Richardson, M.A., Post-White, J., Grimm, E.A., Moye, L.A., Singletary, S.E., & Justice, B. (1997). Coping, life attitudes, and immune responses to imagery and group support after breast cancer treatment. Alternative Therapies in Health and Medicine, 3(5), 62-71.
Roman, J., Olivares, M., Martin, M., & Moreno, A. (2010). Valoracion biopsicosocial en pacientes con patologia mamaria oncologica quirurgica. Psicooncologta, 7(1), 81-97.
Royo, A. (2011). Calidad de vida en pacientes intervenidas de cancer de mama. Trabajo de Investigacion. Barcelona: Universitat Autonoma de Barcelona, Departamento de Medicina Interna. UAB 1, 5-8. Retreived from: http://ddd.uab.cat/pub/trerecpro/2012/hdl_2072_181264/ TR-RoyoAznar.pdf
Sacerdote, P. (1977). Applications of hypnotically elicited mystical states to the treatment of physical and emotional pain. International Journal of Clinical and Experimental Hypnosis, 25(4), 309-324. doi: 10.1080/00207147708415987
Sat-Munoz, D., Contreras-Hernandez, L, Balderas-Pena, L., Hernandez-Chavez, G. A., SolanoMurillo, P, Mariscal-Ramirez, I., Morgan-Villela, G. (2011). Calidad de vida en mujeres mexicanas con cancer de mama en diferentes etapas clinicas у su asociacion con caracteristicas socio-demograficas, estados comorbidos у caracteristicas del proceso de atencion en el Instituto Mexicano del Seguro Social. Value in Health, 14(5), 133-136. doi: 10.1016/j. jval.2011.05.027
Schou, I., Ekeberg, O., Sandvik, L., Hjermstad, M.J., & Ruland, C.M. (2005). Multiple predictors of health-related quality of life in early stage breast cancer: Data from a year follow-up study compared with the general population. Quality of Life Research, 14(8), 1813-1823. doi: 10.1007/sl 1136-005-4344-z
Stanton, H.E. (1990). Dumping the “rubbish”. In D. Corydon (Ed.) Handbook of hypnotic suggestions and metaphors (pp. 313). New York: W.W. Norton and Company.
Tellez, A. (2007). Hipnosis Clinica: Un Punto de Vista Ericksoniano. Mexico: Trillas.
Tellez, A., Garda, C.H., & Corral-Verdugo, V. (2015). Effect size, confidence intervals and statistical power in psychological research. Psychology in Russia: State of the Art, 8(3), 27-46. doi: 10.11621/pir.2015.0303
Tellez, A., Rodriguez, C., Martinez, J., Juarez-Garcia, D., Sanchez-Armaas, O., Sanchez, T, Segura, G & Jaime-Bernal, L. (2017). Psychological Effects of Group Hypnotherapy on Breast Cancer Patients during chemotherapy. American Journal of Clinical Hypnosis, 60(1), 68-84. doi: 10.1080/00029157.2016.1210497
Torem, M.S. (1990). Ego strengthening. In D. Corydon (Ed.) Handbook of hypnotic suggestions and metaphors (pp. 110-112). New York: W.W. Norton and Company.
Uwer, L., Rotonda, C, Guillemin, E, Miny, J., Kaminsky, M. C, Mercier, M. ... Conroy, T. (2011). Responsiveness of EORTC QLQ-C30, QLQ-CR38 and FACT-C quality of life questionnaires in patients with colorectal cancer. Health Quality of Life Outcomes, 9(1), 70. doi: 10.1186/1477-7525-9-70
Vearncombe, K.J., Rolfe, M., Wright, M., Pachana, N.A., Andrew, B., & Beadle, G. (2009). Predictors of cognitive decline after chemotherapy in breast cancer patients. Journal of the International Neuropsychological Society, 15(06), 951-962. doi: 10.1017/S1355617709990567
Watkins, H.H. (1980). The silent abreaction. International Journal of Clinical and Experimental Hypnosis, 28(2), 101-113. doi: 10.1080/00207148008409833
Watkins, J.G. & Watkins, H.H. (1990). Dissociation and displacement: Where goes the “ouch?” American Journal of Clinical Hypnosis, 33(1), 1-10. doi: 10.1080/00029157.1990.10402895
Weaver, K.E., Forsythe, L.P., Reeve, B.B., Alfano, C.M., Rodriguez, J.L., Sabatino, S.A., ... Rowland, J.H. (2012). Mental and physical health-related quality of life among US cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiology Biomarkers & Prevention, 21(11), 2108-2117. doi: 10.1158/1055-9965.EPI12-0740
Wright, M.E. (1987). Clinical practice of hypnotherapy. New York: Guilford Press.
To cite this article: Téllez A., Juárez-García D. M., Jaime-Bernal L., Medina De la Garza C. E., Sánchez T. (2017). The effect of hypnotherapy on the quality of life in women with breast cancer. Psychology in Russia: State of the Art, 10(2), 228-240.
The journal content is licensed with CC BY-NC “Attribution-NonCommercial” Creative Commons license.










