Distress Screening in Russian Pediatric Oncology: Adaptation and Validation of the Distress Rating Scale
Abstract
Background. Children undergoing cancer treatment face a number of emotional, physical, and other problems leading to distress that need to be identified in a timely fashion. Regular assessment of patients’ and their caregivers’ psychosocial health care needs during the patients’ hospital stays has become the standard of psychological care.
Objective. This study was conducted to determine the validity of the Distress Rating Scale (DRS) on a Russian pediatric sample. The DRS appeared to be a reliable pediatric measure of patients’ distress level.
Design. One hundred fifty-nine (159) children of ages 7-17 with cancer and blood disorders, 153 caregivers, and 51 physicians were included in our study. Forty-five families were re-assessed as a test-retest group after a four-week interval. The DRS was validated through the use of the Children's Depression Inventory (CDI) by M. Kovacs and by the Pediatric Quality of Life Inventory (PedsQL 4.0).
Results. The convergent validity of the DRS's Russian version was shown by the reasonable agreement between the children's distress level and standardized measure scores. The criterion validity was demonstrated by significant correlations between the children’s DRS self-reports, and those of their parents and physicians. The robustness and consistency of the results in the primary and repeated assessments between the DRS, the CDI, and the PedsQL, proved the reliability of the scale. Age-specific cut-off scores were determined.
Conclusion. The Russian version of the DRS is a valid tool for rapid and reliable assessment of children’s emotional distress in order to identify their needs for psychological assistance in a timely manner.
Received: 10.03.2019
Accepted: 26.06.2020
Themes: Clinical psychology
PDF: http://psychologyinrussia.com/volumes/pdf/2020_3/Psychology_3_2020_2-17_Nikolskaya.pdf
Pages: 2-17
DOI: 10.11621/pir.2020.0301
Keywords: oncology; pediatric; distress; screening; thermometer; validation; psychological adjustment, Distress Rating Scale (DRS)
Introduction
Children undergoing treatment from oncological and hematological diseases face a number of psychophysical and psychosocial problems associated not only with a life-threatening disease itself, but also with serious, often traumatic, treatment. Treatment is usually accompanied by various side effects, uncomfortable procedures and pain, and a long-term hospitalization with isolation from family and home that leads to the emotional distress of both patients and caregivers (Kazak & Noll, 2015; Khain, 2004; Khain et al., 2014 a; Pai et al., 2007).
It turns out that more than 50% of cancer patients have high distress during their treatment (Dolgin, et al., 2007; Enskar & von Essen, 2007; Holland & Bultz, 2007; Stevens et al., 2006). The traumatic experience of having cancer places children at even more significant risk for distress and psychological maladjustment than adults. It has been noted that childhood cancers could be considered generally distressing for children and their families (Aralova et al., 2016; Kazak & Noll, 2015; Khain & Kholmogorova, 2017; Klipinina & Enikilopov, 2016). As for adolescents, it has been determined that the disruption caused by the cancer experience is probably in part responsible for the significant distress they experience during critical life-stages (Sansom-Daly & Wakefield, 2013). We know that the elevation of emotional distress in families is associated with a number of negative consequences: the decrease of the quality of life in different aspects, the dissatisfaction with the treatment, and low adherence to prescriptions (Kennard et al., 2004).
For these obvious reasons, screening for emotional distress is becoming more common in pediatric cancer care. Moreover, regular assessment and monitoring of children’s and their caregivers’ psychosocial health care needs during cancer treatment has become the standard of psychological care. Such screening is important not only for timely detection of the distress itself, but also to identify those psychosocial problems that interfere with psychological adaptation to treatment(Kazak et al., 2015; Wiener, Viola, Koretski, Perper, & Patenaude, 2015).
Psycho-oncology as an interdisciplinary practice and study is quite a new field in Russia. Clinical psychologists have only recently begun to appear in Russian hospitals, and usually their number is not numerous (Khain et al., 2014 a).Still, there is a lack of psychosocial standards of care as a part of routine medical care, and the criteria for successful adjustment to life-threatening diseases have not yet been determined(Khain et al., 2014 b). Usually, the decision to offer psychological support is guided by a physician’s understanding of a family’s needs, but the degree of that understanding may vary from doctor to doctor. Requests from patients and caregivers for psychological counselling are not common in Russia, where often psychological care is associated with stigmatization.In general, the tradition of discussing psychosocial problems in children with severe diseases has just begun.
Regular assessment and monitoring of children’s and caregivers’ psychosocial health care needs during cancer treatment has become the standard of psychological care. It is helpful not only for timely detection of the distress itself, but also to identify those psychosocial problems that interrupt psychological adjustment to treatment (Holland & Bults, 2007; Varni, Burwinkle, Katz, Meeske, & Dickinson, 2002).
The term “distress” is also not common in Russian. The concept is borrowed from English, and is just now being integrated into professional usage to denote the negative emotional state of cancer patients, gradually replacing the more familiar, but not too specific, everyday concept of “stress.” As in English, the use of a non-stigmatizing word such as “distress” in Russian makes it easier for specialists to begin a dialogue with a family about psychosocial problems, without triggering embarrassment (Holland, Watson, & Dunn, 2011).
The lack of valid tools for assessing and monitoring the child’s and caregiver’s emotional state during treatment limits the further development of Russian psycho-oncology in targeting and providing care in a timely fashion. As a result, psychosocial problems often go unrecognized and without due attention, leading to greater long-term distress.Consideringthe fact that children with cancer can face a number of physical or psychosocial problems caused by their life-threatening disease and harsh treatment, the necessity or advisability of extra attention to emotional distress issues becomes evident. Therefore, there is a great deal of evidence in support of strongly recommending assessments of the psychosocial health care needs of children with cancer and their families (Kazak et al., 2015).
The National Comprehensive Cancer Network (NCCN) distress thermometer (DT)was developed as a screening tool to quickly identify and address emotional distress in cancer adult patients (Holland, 1997). It is widely used to monitor the emotional state of cancer patients (primary diagnosis and follow-up monitoring) (Blenkiron, Brooks, Dearden, & McVey, 2014; Zwahlen, Hagenbuch, Carley, Recklitis, & Buchi, 2008). There is also a pediatric DT, which is considered as a valid, feasible, and acceptable (to children, caregivers, and medical providers) screening tool for sufferers from cancer and other medical illnesses (Patel et al., 2011; Wiener et al., 2017). The validation of the Russian-language version of the children’s DT is a relevant task that may be considered one of the first necessary steps toward developing standardized and targeted psychosocial care in pediatric psycho-oncology.
Methods
Participants
Screening efficacy and the validity of the pediatric Distress Rating Scale was studied on a sample of pediatric patients under treatment at the Dmitry Rogachev National Research Center of Pediatric Hematology, Oncology, and Immunology.
The sample was comprised of patients 7 to 17 years old (n=159) with various cancer disorders (such as blastoma, teratoma, sarcoma, leukemia, and lymphoma), as well as with blood disorders requiring hematopoietic stem cell transplantation (acquired aplastic anemia); their caregivers (n=153); and their physicians (n=51).
Eligibility criteria for patients were hospitalization at the Rogachev Center for inpatient treatment, and native speaker competence in Russian language due to numerous different languages extant in Russia. The use of hematopoietic stem cell transplantation in the treatment of acquired aplastic anemia was identified as the most intense treatment protocol.
Excluded from the study were those children with a psychiatric diagnosis; problematic mental health problems (established earlier, or diagnosed during the cancer treatment); and any concomitant diagnosis or condition which would make it difficult for them to understand the questions or make judgments.
Ethics committee approval was obtained (Approval Number: 2016-217, Local ethics committee and IRB, Federal Research Center for Pediatric Hematology, Oncology, and Immunology, Moscow, Russian Federation). Caregivers and adolescents over 15 years old (according to the law of Russian Federation) provided written informed consent prior to the study.
Procedure
Questionnaires
Distress Rating Scale (DRS)
The Distress Rating Scale (DRS) (Patel et al., 2011) is a developmentally relevant pediatric version of the DT, which was adapted for children with cancer by the Departments of Population Sciences, Pediatrics, and Support Care at the City of Hope. The DRS was adapted for 2-4 year old, 5-6 year old, and 7-17 year old children.
Only the DRS for children and adolescents ages 7 to 17 years appeared to be a valid screening measure to rate a child’s distress. It has a visual analogue scale presented as a thermometer to rate distress level from 0 to 10, and a brief problem checklist (PL).
Patients' distress could be classified on three levels: mild (0-4), moderate (5-7), and severe (8-10). The caregivers received a parent-version of the DRS to rate their perception of their child’s distress, whereas the physicians were asked to fill out a staff-version in order to register the medical team's evaluation. The PL of symptoms that a child may face during the treatment process identifies emotional, physical, practical, spiritual, and family causes for the distress. The child’s, caregiver’s, and physician’s checklist versions consist of a total of 37 symptoms.
Pediatric Quality of Life Inventory 4.0
The PedsQL 4.0 (Varni et al., 2002) is a tool for measuring the health-related quality of life of children and adolescents of ages 2 to 18 years in their physical, emotional, social, and school functioning. Self-report Russian-language versions for children ages 7-17 years (varied for cohorts of 5-7 years, 8-12 years, and 13-18 years), and a Russian-language parent-report version for caregivers were used in order to evaluate the children’s quality of life issues.
Children's Depression Inventory (CDI)
The Children's Depression Inventory (Kovacs, 1992) rates the severity of symptoms related to depression or dysthymic disorder in children and adolescents (from 7 to 17 years old). The CDI yields a total score and five subscales: a) negative mood; b) interpersonal difficulties; c) ineffectiveness; d) anhedonia; and e) negative self-esteem.
The validation study on the Russian-language sample (Volikova, Holmogorova, & Kalina, 2013) showed that the CDI total score (T) could vary from 0 to 54. Fifty (50) was a critical score, after which the depth of symptoms increased. Therefore, we consider the value of T interval ≥ 50 as a critical threshold for diagnosing depression.
The Intensity of Treatment Rating Scale 3.0 (ITR)
The Intensity of Treatment Rating Scale 3.0 (Kazak et al., 2012) is used to assess treatment intensity (ITR-3.0). The ITR-3.0 classifies pediatric cancer treatment on four levels: level 1 = least intense; level 2 = moderately intense; level 3 = very intense; and level 4 = most intense.
Study design
The psychometric characteristics of the DRS have not previously been studied on a Russian-language sample. A validation scheme, using the same elements as the original one, was approved with the consent of the authors.
First, a double-blind translation of the DRS was carried out: peer review was used to select the exact words that most accurately reflect the essence of each statement. Clinical psychologists, as well as oncologists and hematologists, participated as experts in creating a Russian version of the DRS.
Then, several pilot studies were conducted to examine the DRS’s validity for children of three age groups (2-4, 5-6, and 7-17 years old) (Khain & Kholmogorova, 2017; Stefanenko et al., 2017). We encountered the same problems in obtaining valid test results in children under 7 years old as S. Patel and colleagues had (Patel et al., 2011). Children age 2-4 years (n = 18) could not make a clear choice between three faces to rate their level of distress and point to the one that showed how they felt. Children ages 5 to 6 years (n = 10) also had difficulty in filling in both the DRS and the PedsQL due to misunderstanding the questions, and in rating their distress level according to the scale.
A pilot study in a group of patients ages 11-18 years (n = 22) before and after hematopoietic stem cell transplantation (HSCT) demonstrated differences in the distress level before and after the HSCT in adolescents and their parents. In addition, a tendency for the DRS to have convergent validity and test-retest reliability was shown (Khain & Kholmogorova, 2017).
For these reasons, we decided, to go ahead with the validation of the DRS version for children and adolescents ages 7 to 17 years was further examined on the Russian sample of pediatric patients.
A total of 159 patients and 153 caregivers participated in this study. Forty-five families were re-assessed after a four-week interval and comprised a test-retest group (T1 = test, T2 = retest).
Statistical analyses
The XLSTAT-Biomed software was used for all analyses; missing data for variables was left as missing; non-parametric statistical criteria were applied, since no normal distribution of the measured parameters was found. Psychometric characteristics of the DRS were examined.
The Spearman rank (r) correlation analysis was applied to assess the convergent validity, criterion validity, and test-retest reliability of the DRS. Evaluation of convergent validity was conducted by analyzing the correlation between the results of the DRS with the results of standardized child measures for depression (the CDI) and quality of life (the PedsQL). Criterion validity was examined by assessing the connection between a child’s DRS ratings, and the caregivers’ and medical team’s ratings of the patient’s distress. Then test-retest reliability was determined by testing the correlation between the distress ratings and standardized child measures in the test (T1) and retest (T2) groups. Finally, the strength of the correlation between the distress ratings and the problem scores (PL) was studied. Spearman rank correlations were classified as small (< 0.30),moderate (0.30-0.7), and strong (> 0.7). The Mann-Whitney U-test for independent samples was used to study the differences in the distress level in terms of the demographic and clinical characteristics of the sample.
A receiver operating characteristic (ROC) analysis was used to establish a cut-off score for tracing the elevated levels of distress in Russian children with cancer and blood diseases. The area under the ROC curve (AUC) could be > 0.75, 0.5-0.75, or < 0.5, and shows the discriminatory power of the DRS to be high, moderate, or low, respectively. Sensitivity, specificity, and positive or negative predictive values (PPV, NPV) were also examined for every score on the distress scale.
Results
The majority of the children fell within the 13-17 year-old age group (64.8%) (M= 13.5, SD = 2.6). The distribution by gender was almost equal (78 boys and 81 girls). The length of time spent in a medical care setting ranged from 0 to 23 months (M= 13.5, SD = 3.6). Hospitalization was scheduled in 41% of the cases, but 37% of all the pediatric patients were hospitalized for emergency reasons. Approximately 50% of the sample underwent treatment for blood cancer diseases and had ITR scores at the very intense level; 11% had had a relapse. The age range of children’s caregivers was broad, ranging from 28 to 61 years (M= 40.3, SD = 5.5); they were primarily mothers (84%). Of the 120 families who designated their status, 84 were single-parent (52% of the sample). Detailed characteristics of the sample are presented in Figure 1.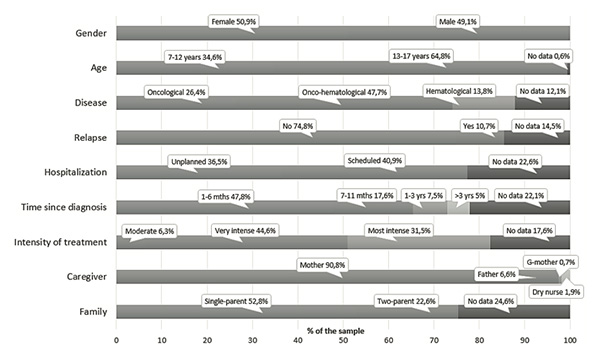
Figure 1.Demographic and clinical characteristics of patients
Note. The diagram illustrates the percentage of the sample by demographic and clinical characteristics.
The convergent validity of the DRS was demonstrated by the reasonable agreement (p < .01, p< .05) between the child's DRS ratings and the standardized measures' scores for depression and quality of life (see Table 1). The children’s distress ratings correlated moderately with their PedsQL total scores (r= -0.538, p< .01), as well as with the CDI total scores (r= 0.332, p< .01), and the CDI subscales. In particular, the thermometer score, and emotional and family/social problem domain scores, moderately correlated (p< .01) with both the Negative Mood (r= 0.240; r= 0.179; r= 0.193), and the Anhedonia (r= 0.438; r= 0.345;r= 0.255) CDI subscales respectively. The physical problem domain scores correlated mildly (p< .01) with the Anhedonia CDI (r= 0.199).
Table 1
Correlation between the child’s DRS ratings and the standardized measures’ scores
|
|
Thermometer score |
Emotional problems |
Physical problems |
Practical problems |
Spiritual problems |
Family/Social problems |
Total score PL (5 domains) |
|
СDI |
|
|
|
|
|
|
|
|
Negative mood |
0.240** |
0.179** |
0.024 |
0.119 |
0.081 |
0.193** |
0.152* |
|
Interpersonal Difficulties |
0.185* |
0.194** |
-0.052 |
0.004 |
0.021 |
0.083 |
0.079 |
|
Ineffectiveness |
0.006 |
0.117 |
0.117 |
0.053 |
0.001 |
0.096 |
0.056 |
|
Anhedonia |
0.438** |
0.345** |
0.199** |
0.111 |
0.125 |
0.255** |
0.342** |
|
Negative Self-Esteem |
0.062 |
0.083 |
-0.053 |
0.009 |
0.027 |
0.058 |
0.022 |
|
Total score CDI |
0.332** |
0.236** |
0.047 |
0.079 |
0.056 |
0.177* |
0.181* |
|
PedsQL |
|
|
|
|
|
|
|
|
Physical functioning |
-0.404** |
-0.299** |
-0.370** |
-0.103 |
-0.101 |
-0.170 |
-0.395** |
|
Emotional functioning |
-0.299** |
-0.431** |
-0.264** |
-0.229* |
-0.128 |
-0.303** |
-0.432** |
|
Social functioning |
-0.430** |
-0.353** |
-0.153 |
-0.129 |
-0.204* |
-0.175 |
-0.307* |
|
School functioning |
-0.291** |
-0.104 |
-0.193* |
-0.437** |
-0.321** |
-0.265** |
-0.300** |
|
Psychosocial Health |
-0.468** |
-0.329** |
-0.212* |
-0.381** |
-0.310** |
-0.270** |
-0.394** |
|
Total score PedsQL |
-0.538** |
-0.424** |
-0.380** |
-0.281** |
-0.221* |
-0.292** |
-0.509** |
Note. * p < .05. ** p < .01.
The DRS’s criterion validity was established by the presence of moderate correlations (p< .01) between the child’s distress score by self-report and the reports of the parents (r= 0.572) and medical team (r= 0.414). Also, there was a statistical connection between all coincident PedsQL scales scores (0.359 ≤ r≤ 0.584) in the child’s and parent’s reports (see Table 2).
The medical team’s ratings of the patients’ distress and accompanying complaints turned out to be moderately correlated (p< .01) with the children’s self-ratings: i.e.,the thermometer scores (r= 0.414); emotional scores (r = 0.340); and physical problem domain scores (r= 0.342). The identification of the children’s spiritual, social, and practical problem domains by the doctors was not sufficiently reliable, which was to be expected due to a physician’s concentration on his or her professional tasks.
Table 2
Correlations of child’ distress and QL self-report with caregiver’ and physician’ratings
|
Patient |
Caregiver |
Physician |
|
DRS |
|
|
|
Thermometer score |
0.572** |
0.414** |
|
Emotional problems |
0.320** |
0.340** |
|
Physical problems |
0.389** |
0.342** |
|
Practical problems |
0.257** |
0.208 |
|
Spiritual problems |
0.497** |
- |
|
Family/Social problems |
0.284** |
0.014 |
|
Total score PL (5 domains) |
0.350** |
0.401** |
|
PedsQL |
|
|
|
Physical functioning |
0.584** |
- |
|
Emotional functioning |
0.447** |
- |
|
Social functioning |
0.359** |
- |
|
School functioning |
0.561** |
- |
|
Psychosocial Health |
0.512** |
- |
|
Total score PedsQL |
0.465** |
- |
Note. ** p < .01
The robustness and consistency of the results in the primary and repeated assessment in the 45 families proved the test-retest reliability of the DRS. The correlations between the DRS (both thermometer scores and PL domains scores) with the CDI and PedsQL total scores in T1 (test-group) and T2 (retest-group) are summarized in Table 3. In both the test and retest samples, the thermometer scores correlated moderately to strongly with the CDI total scores (Т1: r = 0.831, p< .01; Т2: r = 0.623, p< .05), as well as with the PedsQL total scores (Т1: r= -0.527, p< .05; Т2: r = -0.564, p< .05). The total PL scores in all five domains correlated moderately with the CDI total scores (Т1: r= 0.607, p< .05; Т2: r= 0.662, p< .01) and the PedsQL total scores (Т1: r= -0.596,p< .05; Т2: r= -0.538,p< .05).
Table 3
Correlation between the patient’s DRS scores and the standardized measures’ scores at times T1 and T2
|
|
DRS |
|||
|
|
Thermometer score
|
Total score PL (5 domains) |
||
|
СDI |
Т1 |
Т2 |
Т1 |
Т2 |
|
Negative Mood |
0.456 |
0.727** |
0.477 |
0.071 |
|
Interpersonal Difficulties |
0.697** |
0.213 |
0.573* |
0.264 |
|
Ineffectiveness |
0.481 |
0.393 |
0.099 |
0.330 |
|
Anhedonia |
0.698** |
0.480 |
0.552* |
0.830** |
|
Negative Self-Esteem |
0.251 |
0.317 |
0.022 |
0.533* |
|
Total score CDI |
0.831** |
0.623* |
0.607* |
0.662** |
|
PedsQL |
Т1 |
Т2 |
Т1 |
Т2 |
|
Physical functioning |
-0.452 |
-0.345 |
-0.549* |
-0.540* |
|
Emotional functioning |
-0.555* |
-0.598* |
-0.508 |
-0.247 |
|
Social functioning |
-0.295 |
-0.193 |
-0.321 |
-0.310 |
|
School functioning |
-0.436 |
-0.576* |
-0.194 |
-0.571* |
|
Psychosocial Health |
-0.539* |
-0.624* |
-0.442 |
-0.436 |
|
Total score PedsQL |
-0.527* |
-0.564* |
-0.596* |
-0.538* |
Note. * p < .05. ** p < .01.
Correlation analysis showed a significant relationship between the thermometer score and the problem score in all five domains (see Table 4). However, a stronger correlation (moderate) was detected between the thermometer scores and the domains of the emotional and physical problems’ scores (0.412 ≤ r≤ 0.611, p< .01).
Table 4
Correlation between thermometer score and PL domains scores
|
Thermometer score |
|
|
Problem score (PL) |
|
|
Emotional problems |
0.611** |
|
Physical problems |
0.412** |
|
Practical problems |
0.164* |
|
Spiritual problems |
0.225** |
|
Family/Social problems |
0.328** |
|
Total score PL (5 domains) |
0.588** |
Note. * p < .05. ** p < .01.
Establishing the cut-off scores. ROC curve analysis indicated that for the 7-12 year-old agegroup, a DRS cut-off score of 4 providedthe optimal combination of sensitivity (72%) and specificity (66%), for the CDI total depression score higher than 50 T-score (wich is recommended for Russian version of the CDI) (see Table 5). The results for the area under the curve – AUC = 0.709 (SE = 0.068; 95% CI, 0.58-0.84; p= .005) – indicated that we had a good prediction model (see Figure 2).
Table 5
Sensitivity, specificity, PPV, and NPV of DRS ratings in relation to CDI T ≥ 50
in the 7-12 age group
|
Distress rating |
Sensitivity |
Specificity |
PPV |
NPV |
|
0 |
1.000 |
0.000 |
0.48 |
0.00 |
|
1 |
0.862 |
0.344 |
0.54 |
0.73 |
|
2 |
0.793 |
0.437 |
0.56 |
0.70 |
|
3 |
0.759 |
0.500 |
0.58 |
0.70 |
|
4 |
0.724 |
0.656 |
0.66 |
0.72 |
|
5 |
0.655 |
0.750 |
0.70 |
0.71 |
|
6 |
0.241 |
0.906 |
0.70 |
0.57 |
|
7 |
0.138 |
0.969 |
0.80 |
0.55 |
|
8 |
0.069 |
0.969 |
0.67 |
0.53 |
|
9 |
0.034 |
0.969 |
0.50 |
0.53 |
|
10 |
0.000 |
1.000 |
0.00 |
0.52 |
|
10 |
0.000 |
1.000 |
1.00 |
0.48 |
Note. PPV = Positive predictive value. NPV = Negative predictive value.
In the13-17 year-old age group, a cut-off score of 3 on the DRS scale optimally identified 74% of those with depression (sensitivity) and 48% non-depressed (specificity) (see Table 6). The area under the curve – AUC = 0.662 (SE = 0.048; 95% CI, 0.57-0.76; P= .002) – represents a fair prediction model (see Figure 2).
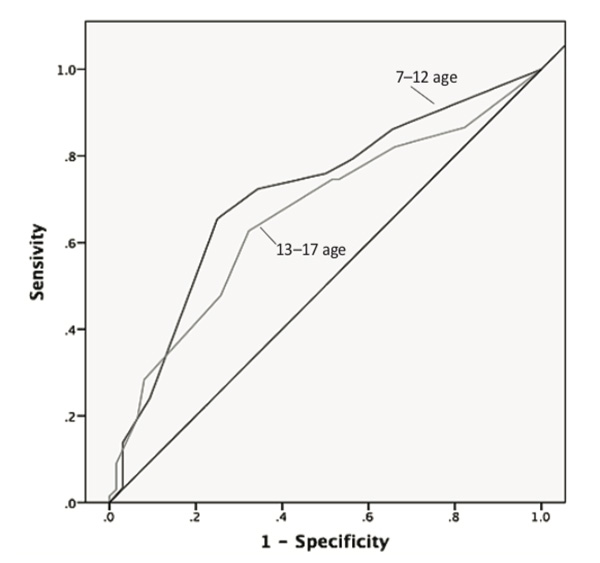
Figure 2. ROC curves of two age groups: 7-12 and 13-17 years (CDI T ≥ 50)
Note. The diagram illustrates the ROC curves for two ages that shows the relationship between sensitivity and specificity for every possible cut-off.
Table 6
Sensitivity, specificity, PPV, and NPV of DRS ratings in relation to CDI T ≥ 50
in the 13-17 age group
Distress rating | Sensitivity | Specificity | PPV | NPV |
0 | 1.000 | 0.000 | 0.52 | 0.00 |
1 | 0.866 | 0.177 | 0.53 | 0.55 |
2 | 0.821 | 0.339 | 0.57 | 0.64 |
3 | 0.746 | 0.484 | 0.61 | 0.63 |
4 | 0.627 | 0.677 | 0.68 | 0.64 |
5 | 0.478 | 0.742 | 0.67 | 0.63 |
6 | 0.284 | 0.919 | 0.79 | 0.57 |
7 | 0.194 | 0.935 | 0.76 | 0.54 |
8 | 0.090 | 0.984 | 0.86 | 0.52 |
9 | 0.030 | 0.984 | 0.67 | 0.50 |
10 | 0.000 | 1.000 | 1.00 | 0.48 |
Note. PPV = Positive predictive value. NPV = Negative predictive value.
Figure 3 presents the differences in the children’s emotional issues depending on the duration of the disease. Patients diagnosed more than three years ago have significantly lower thermometer scores in comparison with patients diagnosed within 0-6 months (U = 259, p= .045), up to 1 year ago (U = 80, p= .007), and 1-3 years ago (U = 26, p= .003). The patients with disease duration of less than three years did not differ in the level of their distress.
Patients who were in treatment for more than six months had a significantly lower PedsQL total score in comparison with those who were in treatment from 0 to 6 months (U = 499, p = .016) (see Figure 3).
At the same time, Figure 3shows that children who have been treated anywhere from 6 months to 3 years, showed a significant increase in Anhedonia over patients who had lived through three years of the disease (U = 39.5, p= .022), and those who started treatment within the last six months (U = 1034, p= .01).
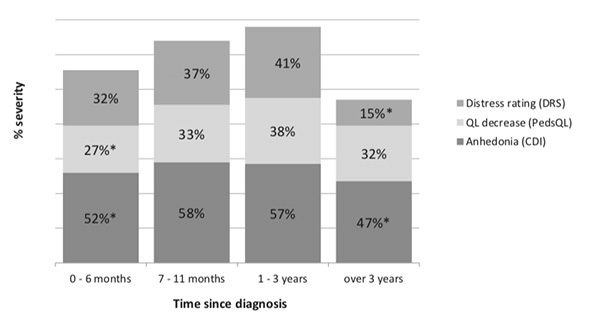
Figure 3. Patients’ emotional issues and time since diagnosis
Note. The histogram illustrates the percentage of severe emotional issues in 4 periods of treatment.*p < .05.
A statistically significant difference in the increase of Anhedonia was also shown when the child’s hospitalization was unplanned (U = 1960, p= .009).
Concerning the child's disease types, there was a significant difference in the PedsQL total score (U = 378.5, p= .006) between those with cancer tumors and those with blood cancer. In particular, children with solid tumors had a significantly lower score on the PedsQL physical activity scale (U = 350.5, p= .002).
As for the types of treatment, patients undergoing chemotherapy showed a significant decrease in their PedsQL total score (U = 90, p= .03). Surgery was accompanied by Anhedonia (U = 1424, p= .019). Children with HSCT had a much greater number of emotional (U = 2385, p= .036) and physical problems (U = 2361, p= .03), as shown by their PL score, as well as depression symptoms: Negative Mood (U = 2174, p= .014), Negative Self-Esteem (U = 1990, p= .002), and Ineffectiveness (U = 1940, p= .001).
Discussion
The purpose of this study was to validate the Russian version of the DRS for children ages 7 to 17 years. The DRS was translated into the Russian language and evaluated on its psychometric properties using data from 159 patients with hematological, onco-hematological, and oncological diseases.The results provided support for convergent and criterion validity, and also demonstrated good test-retest reliability.
The DRS (comprised of the distress thermometer rating and PL) was moderately associated with both the CDI and the PedsQL scores, and indicated good convergent validity; in a test-retest sample of 45 families, the presence of moderate-to-strong correlations between the DRS and the standardized measures proved its robustness and consistency. Criterion validity was confirmed by the moderate correlations between the child’s DRS self-ratings and the ratings of their parents and medical team.
The strongest correlations were found between the children’s overall distress and their emotional and physical problem domains (rather than their spiritual or social problems), which is in accord with findings in other studies. A reliable relationship between the level of distress, and prevalence of emotional and physical problems from the PL, was shown in most instances, but the results on spiritual and religious issues did not look convincing (Iskandarsyah et al., 2013; Jacobsen et al., 2005; Shim, Shin, Jeon, & Hahm, 2008).It seems that during the treatment process, children pay more attention to their physical and emotional state, and present fewer complaints about family, social, or spiritual problems.
The practical problem domain had a small correlation with overall distress. This could be related to the specific conditions at the Rogachev Center during cancer treatment. Children at the hospital have no household duties, and their school problems are mostly solved by having the opportunity to continue their schooling and to get an individualized approach to learningappropriate to their state of well-being during treatment. The thermometer score thus appears sufficient to assess the overall distress level in children. At the same time, the information from the PL can supplement the DT by defining the sources of distress and providing for a more targeted intervention in clinical practice.
We sought age-specified cut-off scores of clinical distress in children ages 7-12 and adolescents ages 13-17. We found that the cut-off score of 4 had optimal sensitivity and specificity relative to the CDI for the children. The cut-off score for adolescents was lower than that for children and was equal to 3. At this level, the sensitivity is high enough not to miss adolescents with problems, although it could result in false-positive cases because of quite low specificity. As a result, every adolescent in need could be offered psychological help. We can assume that the lower cut-off score in adolescents is due to the characteristic tendency for this age group to uphold their personal independence and autonomy and, consequently, hide their emotions. This would be especially true under conditions of invasive treatment, which is often perceived as intrusive and violating not only physical, but also mental boundaries.
As was expected, in different countriesthe distress thermometr also have various cut-off scores (ranged from 3 to 5) for indicating clinically significant problems in emotional well-being, and thus reflect differences among clinical settings, languages, and even cultures (Donovan, Grassi, McGinty, & Jacobsen, 2014). Therefore, the cut-off score of 3 may be due not only to age specificity, but also to a country or cultural characteristic: the strategy of hiding one’s true emotional state and the value of emotional self-control are part of the Russian cultural code. However, this hypothesis requires further study, at least on a Russian adult sample. In fact, the prospect of verifying the cross-cultural validity of the instrument is quite challenging (Bullinger, Anderson, Cella, & Aaronson, 1993).
There was also a significant difference between children’s distress depending upon their different durations of hospitalization. The most difficult period is from six months to three years from the moment of the diagnosis. A possible explanation could be that, on one hand, children who are being forced to undergo treatment far away from home at the Rogachev Center, and lose direct contact with relatives and friends, are more likely to suffer from loneliness; they have a reduced ability to experience pleasant emotions, and a reduced sense of pleasure. On the other hand, by the time fatigue from prolonged and severe treatment accumulates, the children have already managed to get through most phases of their treatment, even though they have not yet completed the entire course of therapy. Also, during this period, followup therapy begins in cases of the ineffectiveness of the first course of treatment, failure to achieve remission, or the detection of an early relapse of the disease.
The results also showed a significant difference in children’s emotional state between treatment types. The children who received HSCT – the most intense treatment (level 4 of treatment intensity) – significantly differed from the others in the number of emotional and physical complaints, as well as depression. This may be due to the fact that for most diseases, the use of such an intense treatment as the HSCT, is supposed to be the “last chance” to achieve remission in the fight against cancer. Thus, these children may have negative self-esteem, and feel depressed and ineffective. Treatment conditions for HSCT are characterized by a higher level of isolation, with less personal space and increasing requirements for compliance with sterility rules in the HSCT Department, so that transplantation becomes one of the most stressful types of treatment (Khain & Kholmogorova, 2017).
Conclusion
The validation of the Russian-language version of the DRS is a relevant task that may be considered one of the first necessary steps towards the development of standardized and targeted psychosocial care in pediatric psycho-oncology in Russia.
The DRS is a reliable pediatric measure of patients’ distress levels in a Russian sample, regardless of their demographic (sex, age) and clinical characteristics (diagnosis, treatment stage, and duration of the disease). As expected, findings from this study revealed no differences in the level of distress by sex (boys and girls), by age (two age groups), by family/caregiver characteristics, or by the disease and the presence of relapse. DT studies have also found no links between the level of distress and the socio-demographic and clinical characteristics of adult patients (Iskandarsyah et al., 2013; Shim et al., 2008).
Limitations
The current study had several limitations that must be noted. It would be useful to conduct future studies with larger sample sizes, especially of physicians. Determining the validity of the DRS criteria seems to be quite challenging. First, despite the fact that our study showed significant correlations between the children’s self-report and parental reports on a child’s distress, the question of using a parental report as a valid proxy for a child report remains controversial and requires further study. Parental reports are likely to be influenced by their own emotional state (Abate et al., 2018). Second, relying on medical team reports on a child’s distress, rather than on a psychosocial specialists’ expert opinion, somewhat limits the ability of our study to achieve a reliable evaluation of the validity of the DRS criteria.
Acknowledgements
We would like to thank all the children and parents who participated in this study. In addition, we wish to thank the medical staff for their cooperation. Furthermore, we would like to thank Regina Pirumova for her help with the DRS Russian translation, Alexey Smirnov for the data collection, Kirill Voronin for supporting the study with statistical analyses, and Marat Kazanov for his help with the English translation of this paper.
References
Abate, C., Lippé, S., Bertout, L., Drouin, S., Krajnovic, M., Roundeau, E., … Sultan, S. (2018). Could we use parent report as a valid proxy of child report on anxiety, depression, and distress? A systematic investigation of father-mother-child triads in children successfully treated for leukemia.Pediatric Blood Cancer, 65(2), e26840. https://doi:10.1002/pbc.26840.
Aralova, M., Robertson, E., Putrya, A., Goncharova, L., Wakefield, C., & Aslanyan, K. (2016). Relationships between Russian mothers and their children with, and without, cancer: A controlled study. International Journal of Healthcare,2(2), 73–80. http://dx.doi.org/10.5430/ijh.v2n2p73.
Blenkiron, P., Brooks, A., Dearden, R., & McVey, J. (2014). Use of the distress thermometer to evaluate symptoms, outcomes, and satisfaction in a specialist psycho-oncology service. General Hospital Psychiatry, 36(6), 607–612. https://doi:10.1016/j.genhosppsych.2014.06.003.
Bullinger, M., Anderson, R., Cella, D., & Aaronson, N. (1993). Developing and evaluating cross-cultural instruments from minimum requirements to optimal models. Quality of Life Research, 2, 451–459. https://doi.org/10.1007/BF00422219.
Dolgin, M., Phipps, S., Fairclough, D., Sahler, O., Askins, M., Noll, R., … Katz, E. (2007). Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history investigation. Journal of Pediatric Psychology,32(7), 771-782. https://doi.org/10.1093/jpepsy/jsm013.
Donovan, K., Grassi, L., McGinty, H., & Jacobsen, P. (2014). Validation of the distress thermometer worldwide: state of the science. Psycho-Oncology,23(3), 241–250. https://doi.org/10.1002/pon.3430.
Enskär, K., & von Essen, L. (2007). Prevalence of aspects of distress, coping, support and care among adolescents and young adults undergoing and being off cancer treatment. European Journal of Oncology Nursing,11(5), 400–408. https://doi.org/10.1016/j.ejon.2007.01.003.
Jacobsen, P., Donovan, K., Trask, P., Fleishman, S., Zabora, J., Baker, F., & Holland, J. (2005). Screening for psychologic distress in ambulatory cancer patients. Cancer, 103(7), 1494–1502. https://doi.org/10.1002/cncr.20940.
Holland, J. (1997). Preliminary guidelines for the treatment of distress. Oncology(Williston Park), 11(11А), 109–114.
Holland, J., Watson, M., & Dunn, J. (2011). The IPOS New International Standard of Quality Cancer Care: integrating the psychosocial domain into routine care. Psycho-Oncology, 20(7), 677–680. https://doi.org/10.1002/pon.1978.
Holland, J., & Bultz, B. (2007). The NCCN guideline for distress management: a case for making distress the sixth vital sign. The Journal of the National Comprehensive Cancer Network, 5(1), 3–7.
Iskandarsyah, A., de Klerk, C., Suardi, D., Soemitro, M., Sadarjoen, S., & Passchier, J. (2013). The Distress Thermometer and its validity: a first psychometric study in Indonesian women with breast cancer. PLOS ONE, 8(2), e56353. http://doi.org/10.1371/journal.pone.0056353.
Kazak, A., Abrams, A., Banks, J., Christofferson, J., DiDonato, S., Grootenhuis, M, … Kupst, M. (2015). Psychosocial Assessment as a Standard of Care in Pediatric Cancer. Pediatric Blood and Cancer, 62(5), 426–459. https://doi.org/10.1002/pbc.25730.
Kazak, A., Hocking, M., Ittenbach, R., Meadows, A., Hobbie, W., DeRosa, B., … Reilly, A. (2012). A Revision of the Intensity of Treatment Rating Scale: Classifying the Intensity of Pediatric Cancer Treatment. Pediatric Blood and Cancer, 59(1), 96–99. https://doi.org/10.1002/pbc.23320.
Kazak, A., & Noll, R. (2015). The integration of psychology into pediatric oncology research and practice: collaboration to improve care and outcomes for children and families.American Psychologist, 70(2), 146–158. http://dx.doi.org/10.1037/a0035695.
Kennard, B., Smith, S., Olvera, R., Bawdon, R., O'hAilin, A., Lewis, C., & Winick, N. (2004). Nonadherence in adolescent oncology patients: preliminary data on psychological risk factors and relationships to outcome. Journal of Clinical Psychology in Medical Settings, 11(1), 31–39. https://doi.org/10.1023/B:JOCS.0000016267.21912.74.
Khain, A. (2014) Psychological adjustment to hematopoietic stem cell transplantation in adolescents: individual and family factors. Konsul'tativnaya psikhologiya i psikhoterapiya [Counseling Psychology and Psychotherapy],25(2), 94–114. https://doi.org/10.17759/cpp.2017250206
Khain, A., & Kholmogorova, A. (2017). Family factors of psychological adjustment to stress in adolescents and their mothers undergoing hematopoietic stem cell transplantation (HSCT). RSUH/RGGU Bulletin Series: Psychology. Pedagogics. Education, 4, 75–97. https://doi:10.28995/2073-6398-2017-4-75-97
Khain, A., Klipinina, N., Kudryavitsky, A., Nikolskaya, N., Stefanenko, E., & Evdokimova, M. (2014, a). Psychosocial adaptation of children with severe somatic diseases to therapy. Pediatric Hematology/Oncology and Immunopathology, 13, 56–62.
Khain, A., Klipinina, N., Nikolskaya, N., Orlov, A., Evdokimova, M., Stefanenko, E., & Kudryavitsky, A. (2014, b). The practical aspects of setting up and operating a psychological service in pediatric oncology/hematology. Konsul'tativnaya psikhologiya i psikhoterapiya [Counseling Psychology and Psychotherapy],22, 106–126.
Klipinina, N., & Enikolopov, S. (2016). Contemporary directions of parental distress investigations during the child’s treatment of life-threatening diseases. V.M. Bekhterev Review of Psychiatry and Medical Psychology, 1, 29–36.
Kovacs, M. (1992). The Children’s Depression Inventory (CDI) manual. North Tanawanda, New York: Multi-Health Systems.
Pai, A., Greenley, R., Lewandowski, A., Drotar, D., Youngstrom, E., & Peterson C. (2007). A meta-analytic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology, 21(3), 407–415. https://doi:10.1037/0893-3200.21.3.407.
Patel, S., Mullins, W., Turk, A., Dekel, N., Kinjo, Ch., & Sato, J. (2011). Distress screening, rater agreement, and services in pediatric oncology. Psycho-Oncology, 20(12), 1324–1333. https://doi:10.1002/pon.1859.
Sansom-Daly, U., & Wakefield, C. (2013). Distress and adjustment among adolescents and young adults with cancer: an empirical and conceptual review.Translational Pediatrics, 2(4), 167–197. https://doi:10.3978/j.issn.2224-4336.2013.10.06.
Shim, E., Shin, Y., Jeon, H., & Hahm, B. (2008). Distress and its correlates in Korean cancer patients: pilot use of the distress thermometer and the problem list. Psycho-Oncology, 17(6), 548–555. https://doi:10.1002/pon.1275.
Stefanenko, E., Nikolskaya, N., Khain, A., Klipinina, N., Riabova, T., Smirnov, A., … Balakhneva, A. (2017).Initial validation of the distress rating scale among Russian pediatric oncology patients and caregivers. Psycho-Oncology, 26(3), 150. https://doi.org/10.1002/pon.4878.
Stevens, B., McKeever, P., Law, M., Booth, M., Greenberg, M., Daub, S., … Epstein, I. (2006). Children receiving chemotherapy at home: Perceptions of children and parents. Journal of Pediatric Oncology Nursing, 23(5), 276–285.https://doi.org/10.1177/1043454206291349.
Varni, J., Burwinkle, T., Katz, E., Meeske, K., & Dickinson, P. (2002). The PedsQL™in pediatric cancer: Reliability and validity of the Pediatric Quality of Life Inventory™Generic Core Scales, Multidimensional Fatigue Scale, and Cancer Module.Cancer, 94(7), 2090–2106. https://doi:10.1002/cncr.10428.
Volikova, S., Holmogorova, A., & Kalina, O (2013). Metodicheskie rekomendacii: Primenenie oprosnika detskoj depressii. M. Kovak (CDI). Moscow:FGBU “MNIIP”.
Wiener, L., Viola, A., Koretski, J., Perper, E., & Patenaude, A. (2015). Pediatric psycho-oncology care: standards, guidelines, and consensus reports. Psycho-oncology, 24(2), 204–211. https://doi:10.1002/pon.3589.
Wiener, L., Battles, H., Zadeh, S., Widemann, B.C., & Pao, M. (2017). Validity, specificity, feasibility, and acceptability of a brief pediatric distress thermometer in outpatient clinics. Psycho-oncology, 26(4), 461–468. https://doi:10.1002/pon.4038.
Zwahlen, D., Hagenbuch, N., Carley, M., Recklitis, C., & Buchi, S. (2008). Screening cancer patients' families with the distress thermometer (DT): a validation study. Psycho-oncology, 17(10), 959–966. https://doi.org/10.1002/pon.1320
To cite this article: Nikolskaya, N.S., Khain, A.E., Stefanenko, E.A., Riabova, T.V., Klipinina, N.V., Shutkova, E.S. (2020). Distress Screening in Russian Pediatric Oncology: Adaptation and Validation of the Distress Rating Scale. Psychology in Russia: State of the Art, 13(3), 35-50.
The journal content is licensed with CC BY-NC “Attribution-NonCommercial” Creative Commons license.









